






Dry AMD can be asymptomatic in its early stages, but it can also eventually show in a dark spot in your central vision. Even when this spot is very small and light, it may be wise to address the situation quickly to avoid it taking more of your central vision.
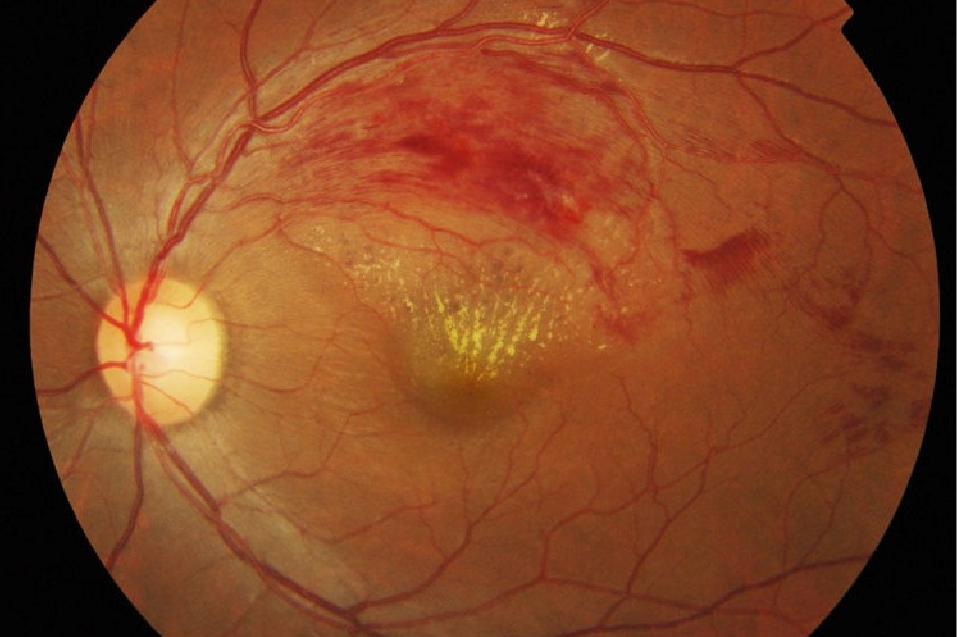
Wet AMD symptoms are generally related to abnormal or distorted central vision. For instance, when looking at a grid of straight lines, you may find the central line in your view wavy. Blurry or dark central vision can also be a symptom of wet AMD.
These symptoms can worsen over time and can lead to irreversible vision loss if untreated. This is why it is generally advised to get screened for and potentially treat wet AMD once such signs appear.
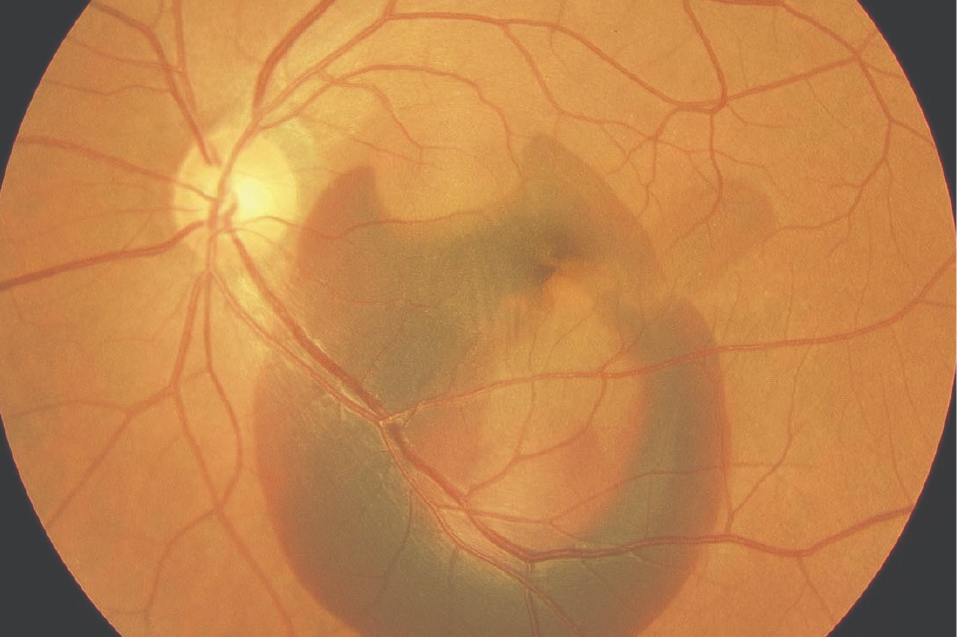
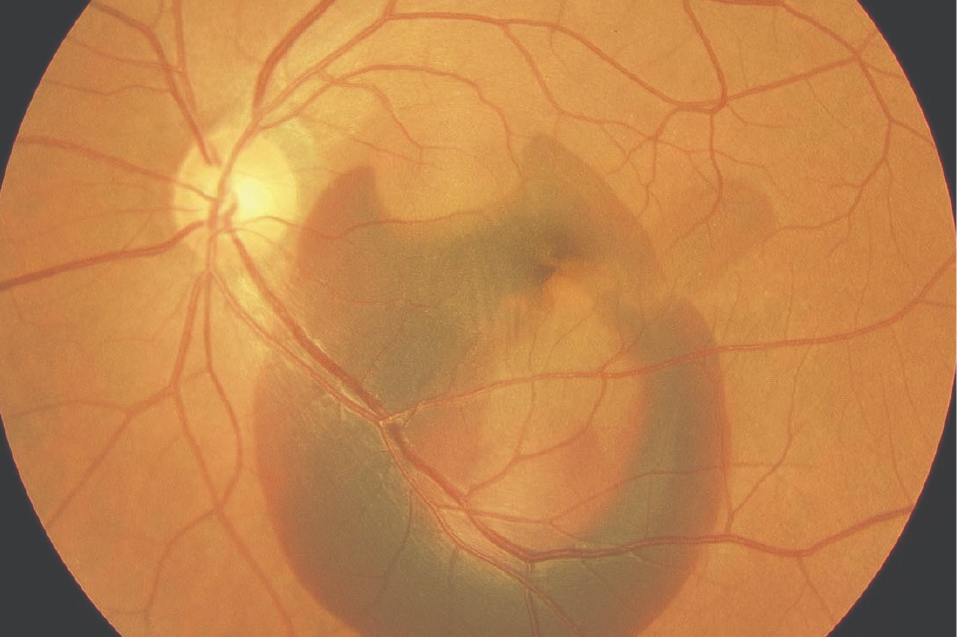
Central serous chorioretinopathy symptoms may include blurry central vision, distortion of straight lines, and micropsia, where an object looks smaller or more distant to an affected eye than to a normal one. However, CSC can also be asymptomatic if the affected areas lie outside of the macula.
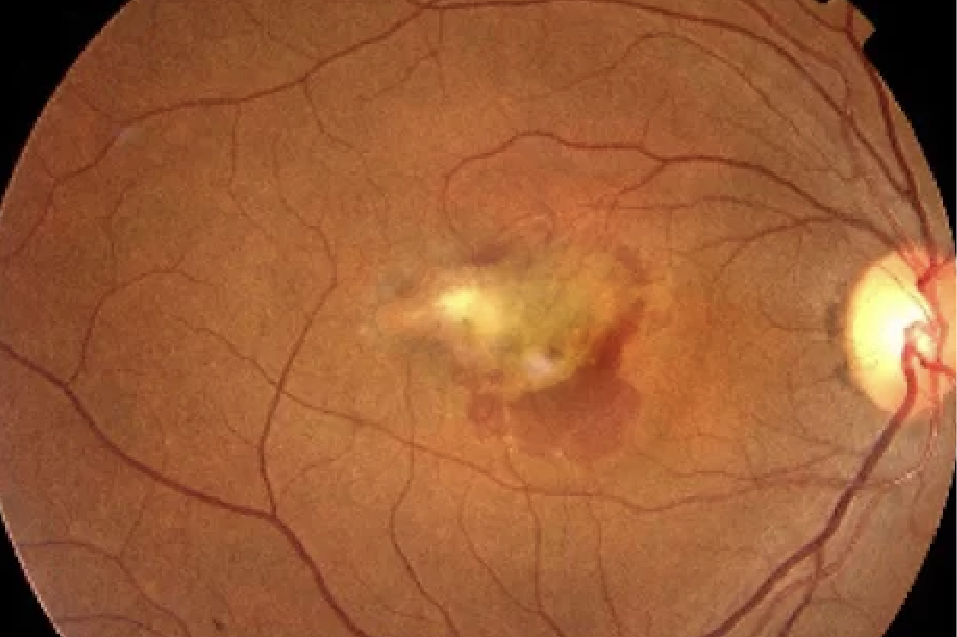
The symptoms of PCV include blurry vision or partial blind spots, usually near the centre of your vision. Scotoma or an abnormally distorted part of otherwise clear vision is another common symptom. Severe cases of PCV may result irreversible scarring and loss of central vision if left untreated.
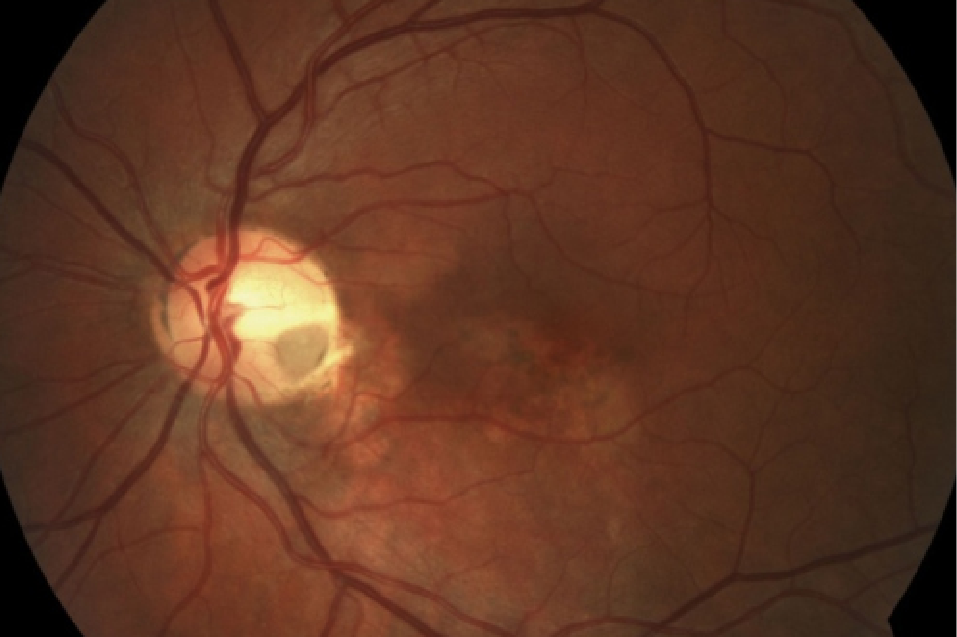
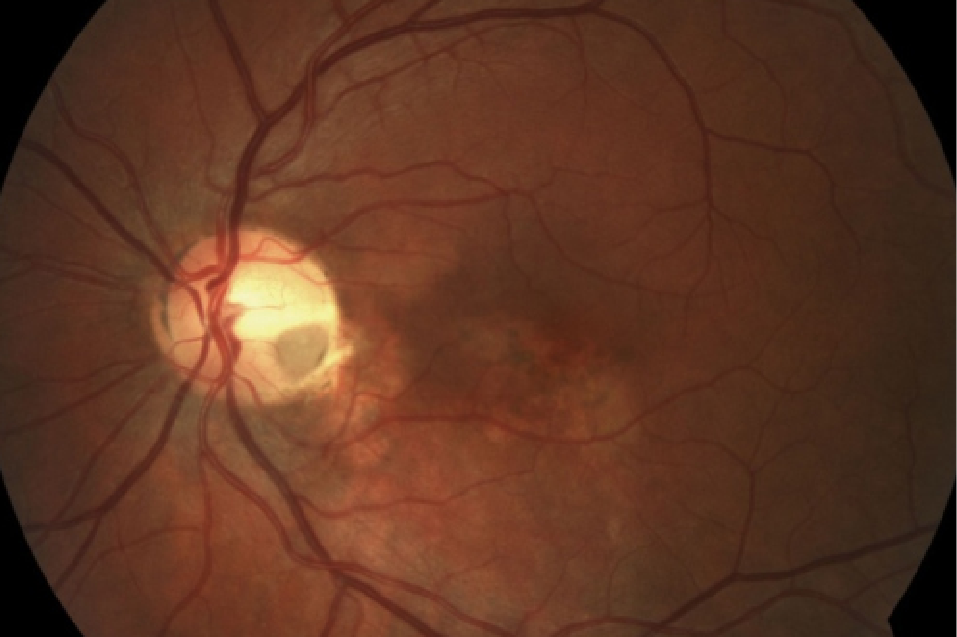
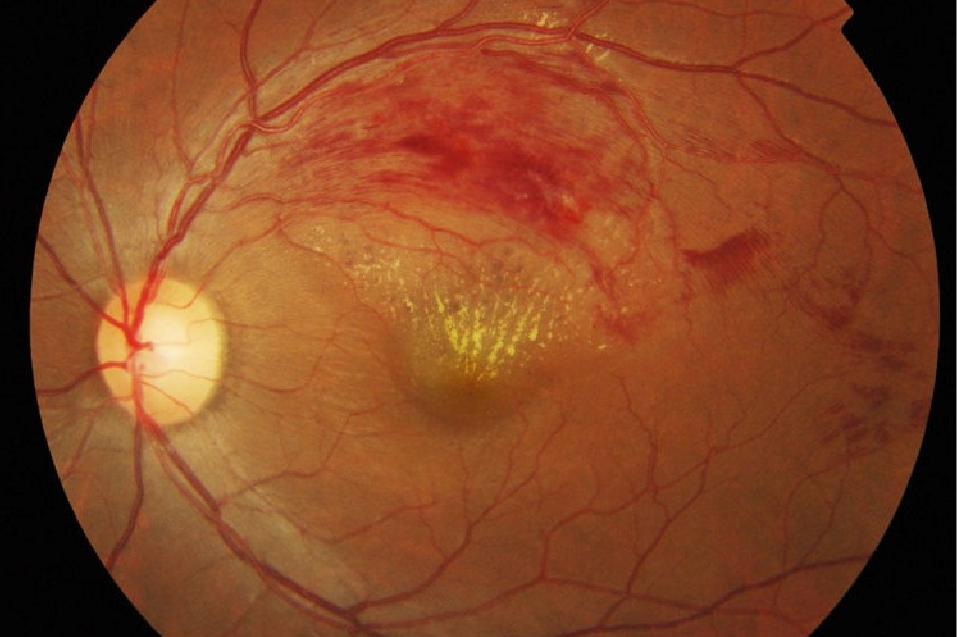
The symptoms of RVO depend on the severity of the blockage of the affected retinal vein. Milder cases may be asymptomatic, while partial or serious vision loss may occur in more severe cases of RVO.
Here are some of the most common symptoms of RVO:
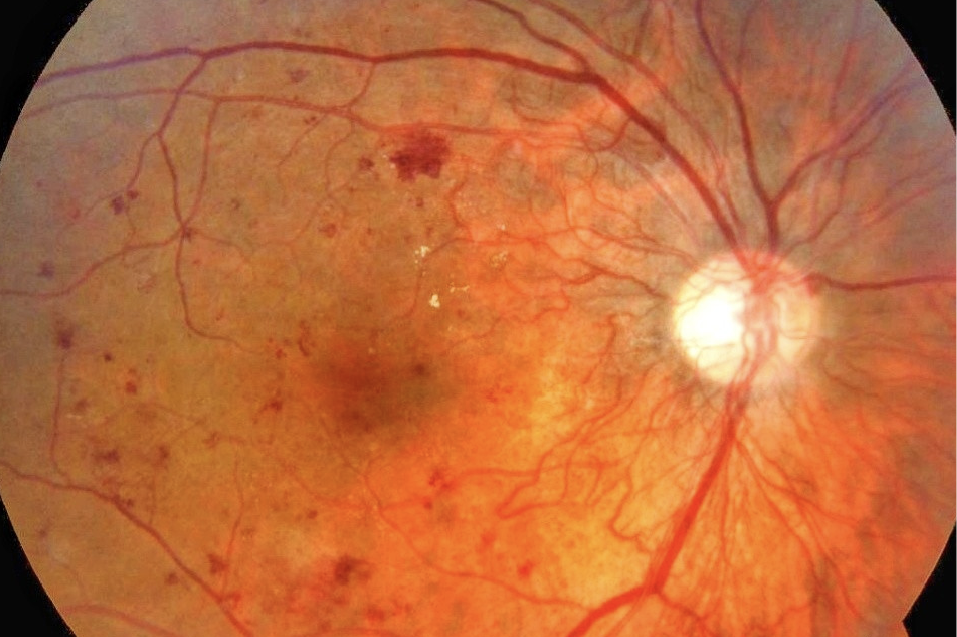
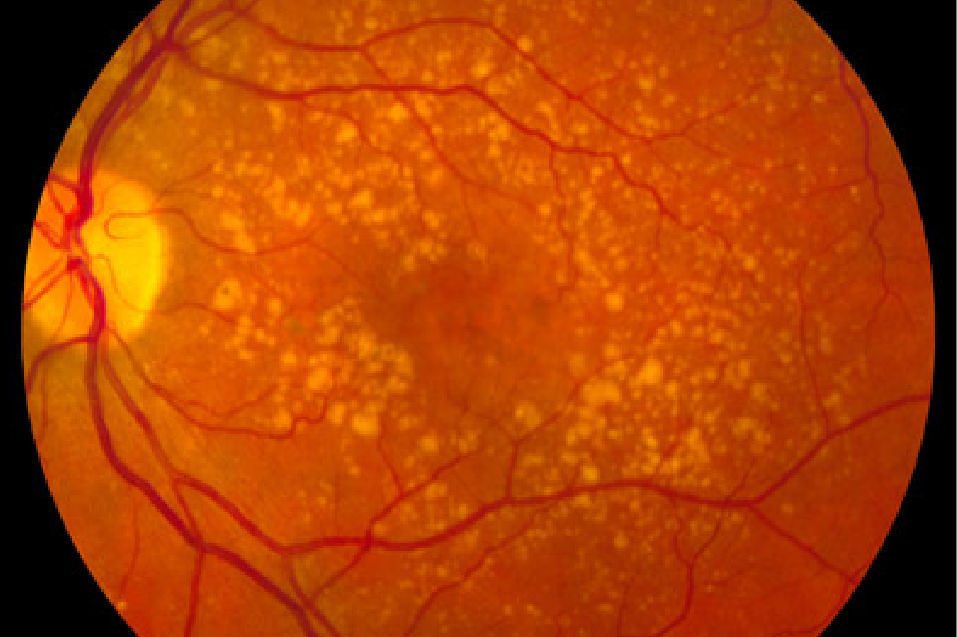
This condition often has no symptoms in its early stages. As it progresses, diabetic retinopathy may cause:
Tests performed during eye screening examinations for retinal issues include Amsler grid, careful dilated eye examination, fluorescein & indocyanine green angiography, and optical coherence tomography (OCT).
If available, it’s best to bring any results of previous tests and records of your medical history for your appointment.
The amount of time it takes to get results from an eye screening will vary. Each case is treated on an individual bases for thoroughness.
Recovery periods vary based on your unique circumstances and the condition and treatment applicable. For example, the usual recovery period for an anti-VEGF injection for wet AMD is usually as short as several days. Meanwhile, the recovery for a vitrectomy for an RVO-related haemorrhage could take several weeks.
Each patient is unique and your doctor can assess your case to determine how many treatments you require. Most patients with wet AMD start at 3 injections every 4 weeks, but it always varies on a case-to-case basis.
RVO can be managed, especially its side effects (like vision loss). The occlusion itself cannot be treated, however.