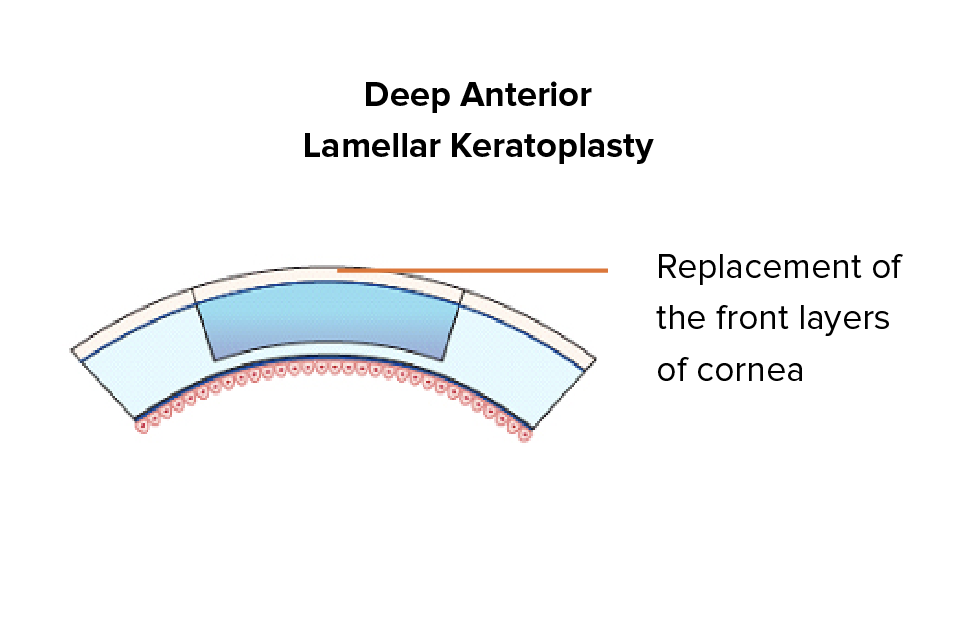
ALK is a type of lamellar keratoplasty that allows the surgeon to preserve the endothelium, which is the innermost layer of the cornea. The front layers of the cornea are the ones replaced instead, as in Deep Anterior Lamellar Keratoplasty or DALK.
The chief benefit of this approach is that corneal transplant rejection is brought down even further, reaching a risk as low as 1-2%. It also translates to a lower chance of complications after surgery, and high suitability for cases where there are superficial corneal scars or keratoconus. This procedure can be more difficult to perform for the surgeon.
EK is called for when the opacity or abnormality in the cornea is in its innermost layer, called the endothelium. In an EK procedure, the front or outermost layers are left as they are and the innermost layers are the ones replaced.
This is a sutureless surgery where the donor endothelium is inserted through a tiny side incision in the eye, translating to faster recovery. It can even be performed as a day surgery and under local anaesthetics. EK surgeries also have very low transplant rejection rates, at just 1-8%.
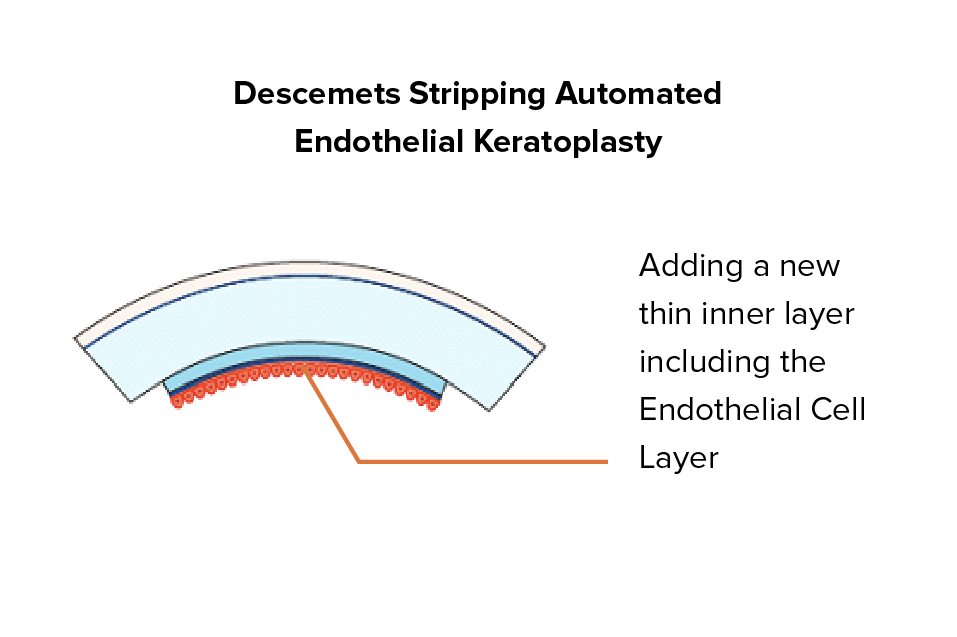
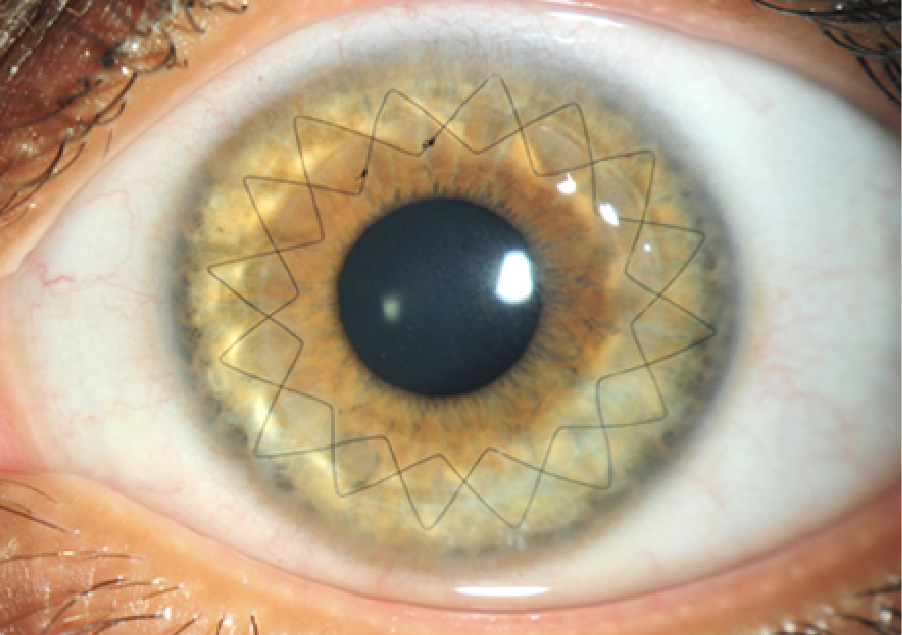
Those seeking DSAEK surgery in Singapore generally do so for an automated version of the partial-thickness corneal transplant. With this procedure, a microkeratome dissects the donor cornea pre-transplant. It has lower transplant rejection rates than PK, and is a fairly common procedure nowadays.
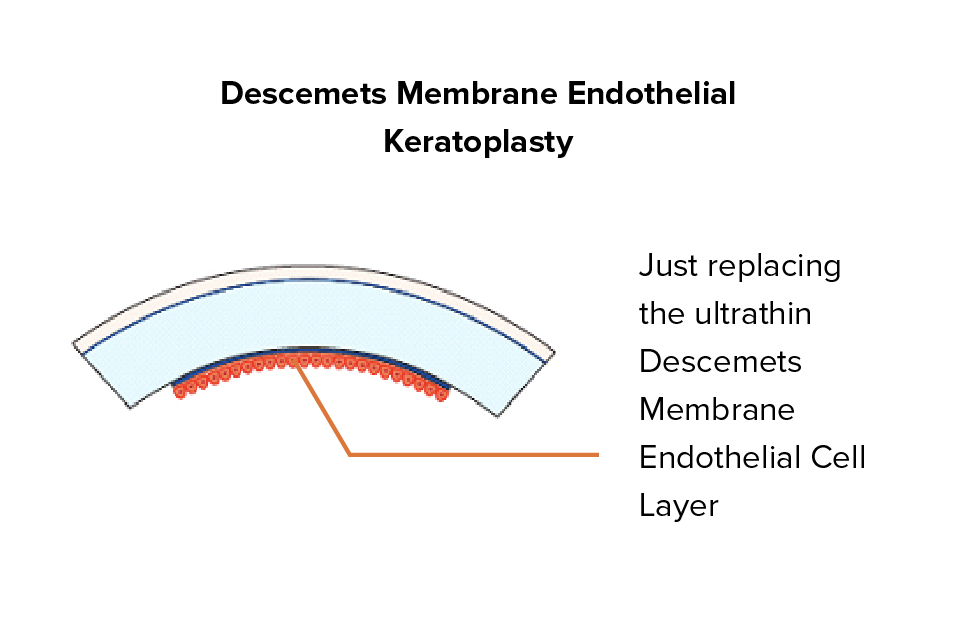
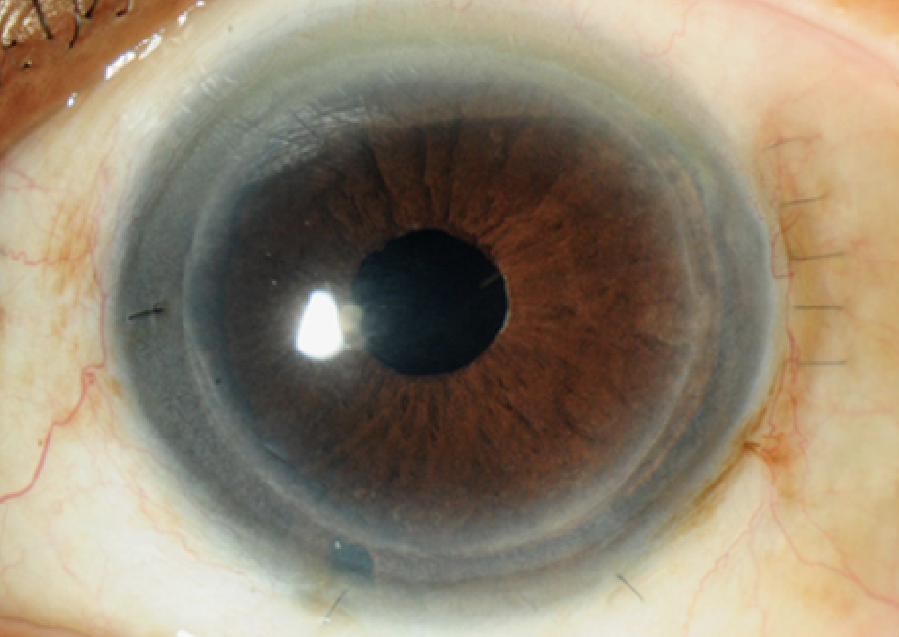
DMEK surgery in Singapore is another version of the partial-thickness corneal transplant surgery. It differs from DSAEK by using an even thinner graft of just 5 to 10 microns, making it both more difficult to execute, but less likely to result in a transplant rejection. It also offers high vision improvement outcomes in most cases.
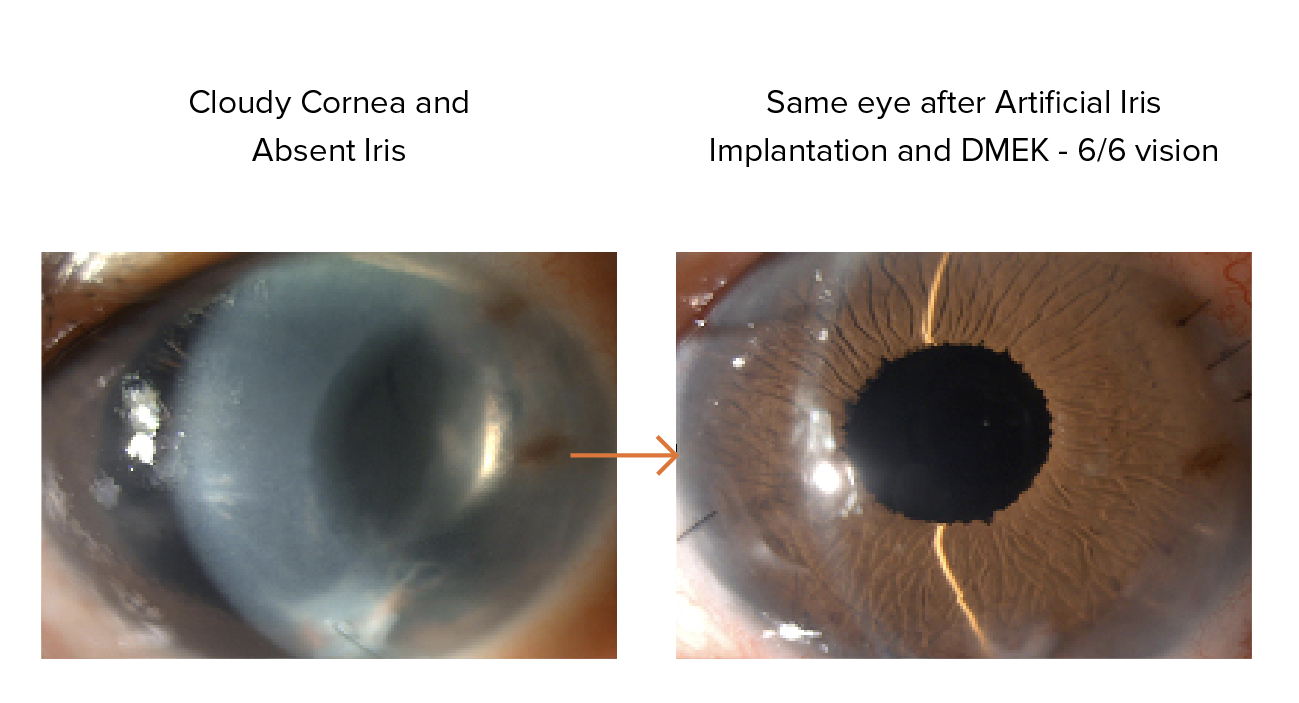
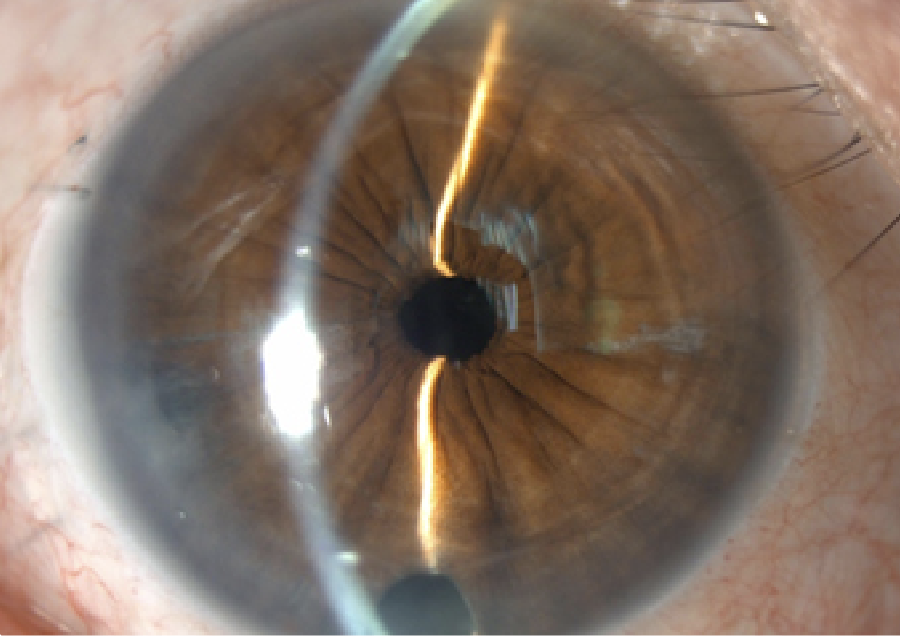
Artificial iris surgery is a relatively uncommon procedure that may be combined with corneal surgery for some patients with iris defects. Because of the iris’s placement behind the cornea, an abnormal one may sometimes end up stuck to the rear of the corneal graft. This can damage the cornea and even heighten the odds of transplant rejection.
An artificial iris can now be used to replace damaged pupils or irises during a corneal transplant, however. This renders procedures like DMEK feasible even in cases where the iris would have previously made them difficult or unlikely to succeed.

The Boston type I keratoprosthesis is an artificial cornea made of titanium and plastic. Because it is not living tissue, it carries no risk of rejection, although it has other risks such as secondary infection and glaucoma development.
The risks for this corneal prosthetic are higher than they are for other corneal transplants. As a result, this is usually chosen only after an actual transplant has been deemed unsuccessful or highly unlikely to succeed.

The osteo-odonto keratoprosthesis procedure is one that requires a two-stage process. Here, part of one of the patient’s teeth is extracted along with an alveolar bone.
This is then used as the supporting structure for an artificial cornea. This is another option reserved for more severe corneal issues where the other transplantation and artificial corneas have failed or are likely to fail. This is a rare procedure as well, to the point where not all countries offer it.
Corneal surgery is typically not painful because anaesthesia is used to numb the area during the procedure. Some discomfort or tenderness may be felt after the procedure, however.
The amount of time it takes to recover from a corneal transplant varies based on the patient’s circumstances and the specific transplant procedure performed. Most people achieve complete recovery and vision improvement 12 months later.
Most patients need to wait only a few weeks for a corneal transplant donor in Singapore, as ERS Suntec City procures corneas from a wide variety of sources. These include local and international eye banks.
Most cornea transplant procedures are completed in 1 to 2 hours.
Cornea transplants can have several risks, the chief one being transplant rejection. Other risks include infection and a higher chance of developing glaucoma post-transplant.